Treatment Of Tuberculosis
Combination therapy and good adherence are the foundations of tuberculosis treatment. Learn more about the methods to cure this disease that are applied today.

Tuberculosis has been a deadly disease for centuries. However, with the passage of time and advances in medicine, the incidence of infection has been slowly declining. If you are interested in knowing more about it, keep reading, because below we will delve into the treatment of tuberculosis.
In the late 1940s, the discovery of streptomycin began to lay the foundation for effective tuberculosis treatment. This treatment would be progressively improved thanks to the findings of isoniazid, rifampicin and ethambutol during the 1960s.
Fortunately, the picture continues to improve and tuberculosis has become a treatable disease.
According to what was stated in the 2019 report of the World Health Organization:
What is tuberculosis?
Tuberculosis is an infectious disease caused mainly by the bacteria called Mycobacterium tuberculosis . This bacterium is also known as “Koch’s bacillus” and constitutes, together with M. bovis and M. africanum, the Mycobacterium tuberculosis complex group .
The human being is the only depository of this microorganism ; Hence, it can be fatal if treatment is not prescribed in time.
The disease is transmitted by close contact from one person to another by inhaling infectious aerosols. Patients who shed bacilli in their respiratory secretions are called bacillifers.
The highest mortality rates are found mainly in countries in Africa and Asia, where living conditions are precarious. This is due to the relationship between tuberculosis pathogens and HIV. In this sense, a quarter of the deaths of patients with HIV are a consequence of tuberculosis.
Treatment of tuberculosis
The therapeutic approach to tuberculosis consists of two types of drugs, although to prevent the development of resistance they are usually associated:
- First-line drugs comprise the quintessential tuberculosis treatment. They are isoniazid, rifampin, rifabutin, ethambutol, and pyrazinamide.
- Second-line drugs are used to treat infections in which resistance to the former drugs is suspected or when the latter give problems due to the appearance of adverse reactions. Capreomycin, cycloserine, streptomycin, clarithromycin, and ciprofloxacin stand out.
Phases of treatment
The most widely used action strategy to deal with tuberculosis consists of two phases:
- Initial treatment phase: This stage lasts about 2 months and it combines isoniazid, rifampicin and pyrazinamide. Ethambutol can be added if the body is suspected of being resistant.
- Treatment continuation phase: lasting approximately 4 months, isoniazid and rifampicin are associated with it.
First-line drugs
In the treatment of tuberculosis, the drugs that fall into this category are key. The estimated administration period is 6 to 9 months.
Currently, there are 10 drugs approved for the treatment of tuberculosis, including the following:
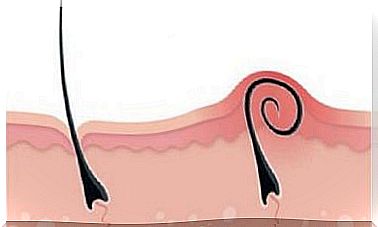
- Isoniazid : This drug prevents the growth of latent microorganisms (that is, it is bacteriostatic), but it also kills active bacteria. Its mechanism of action is based on the inhibition of the synthesis of mycolic acids (constituents of the cell wall of mycobacteria). Its adverse effects are skin rashes, hepatotoxicity, and neuropathies. The latter are a consequence of pyridoxine (vitamin B6) deficiency and are prevented by administering it.
- Rifampicin: it is one of the most active anti-tuberculosis drugs known; it acts by inhibiting the microorganism’s RNA polymerase. It is administered orally and is distributed in the tissues staining saliva, sputum, tears and sweat orange. Adverse effects are rare; they may include skin rashes, fever, and jaundiced liver lesions.
- Ethambutol: this drug should never be used in monotherapy, as resistance quickly appears. Its effect is bacteriostatic, due to the inhibition of the synthesis of the mycobacterial cell wall. Orally administered and well absorbed, only optic neuritis is reported as an adverse effect.
- Pyrazinamide: Like isoniazid, pyrazinamide inhibits the synthesis of bacterial mycolic acids. Adverse effects include gout and liver disease.
Second-line drugs
This group of drugs comes into play in the treatment of first-line drug-resistant tuberculosis. This subtype of tuberculosis is difficult to treat; the most commonly used drugs for these purposes are capreomycin (IM), cycloserine (PO) and streptomycin (IM).
Is there a vaccine for tuberculosis?

The answer to this question is yes. BCG or Bacillus Calmette-Guérin is a vaccine against tuberculosis disease. Generally, its administration is recommended only in certain people who meet very specific criteria and after consulting with an expert.
Ultimately, it is advisable especially in children and health workers who are continuously exposed to the disease. The analysis of a health professional will be essential to indicate it when appropriate.